Oral Health Affects Your Whole Health, but How?
Most people think of oral health as separate from their overall wellbeing, but your mouth serves as a gateway to your entire body. The bacteria and inflammation that develop from poor dental hygiene don’t stay confined to your teeth and gums. They can travel through your bloodstream and trigger serious health complications throughout your system.
Recent research has established compelling connections between periodontal disease and conditions like diabetes, heart disease, Alzheimer’s, and even cancer. Understanding these links can help you take control of both your oral health and your overall wellness.
Cardiovascular Disease: When Your Gums Threaten Your Heart
Your heart and mouth share a dangerous relationship that puts millions at risk every day. When gum disease takes hold, the inflammation and infection create an entry point for harmful bacteria to enter your bloodstream and travel directly to your cardiovascular system.
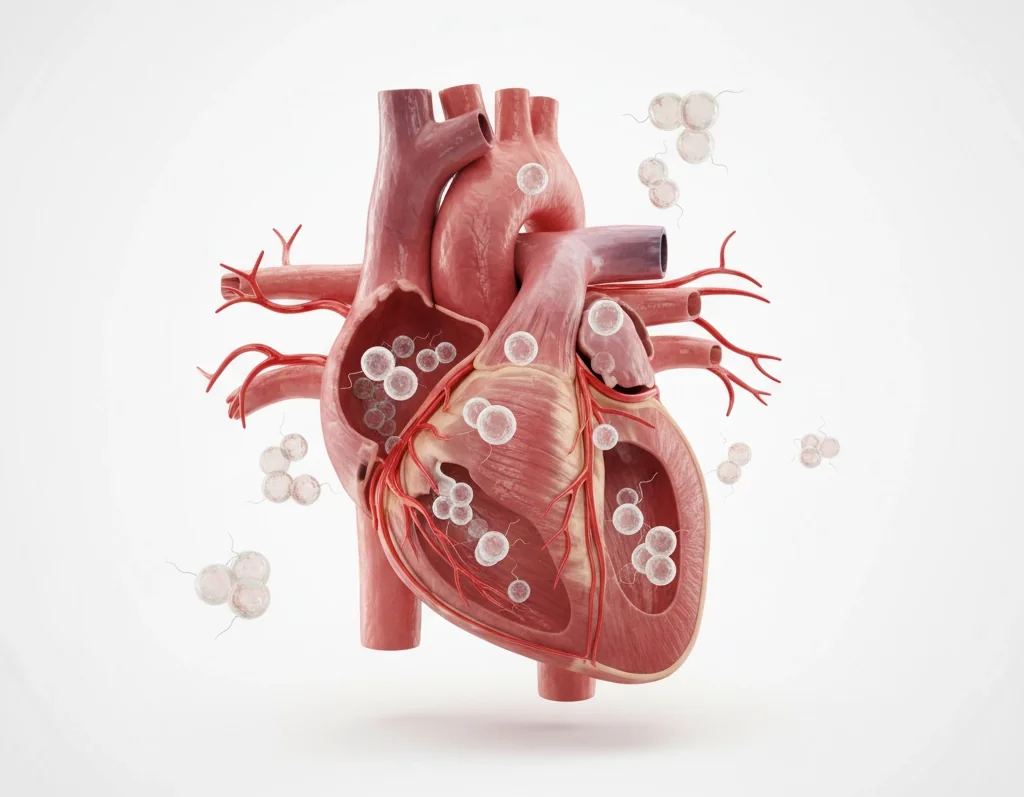
The process works through several mechanisms. First, the chronic inflammation from periodontal disease increases inflammation throughout your entire body, including in your arteries. This systemic inflammation can contribute to the formation of arterial plaques, making heart attacks and strokes more likely.
Additionally, oral bacteria can directly affect your heart through endocarditis. This is an infection of the heart’s inner lining that occurs when bacteria from your mouth enter the bloodstream and attach to your heart’s chambers or valves. This condition can be life-threatening if left untreated.
Studies consistently show that people with gum disease face a significantly higher risk of:
- Heart attack
- Stroke
- High blood pressure
- Arterial disease
The connection is so strong that some cardiologists now recommend dental evaluations as part of heart disease prevention strategies.
Diabetes: A Two-Way Street of Complications
The relationship between oral health and diabetes creates a particularly dangerous cycle where each condition makes the other worse. If you have diabetes, you’re more likely to develop gum disease. Conversely, if you have gum disease, it becomes much harder to control your blood sugar levels.
Here’s how this bidirectional relationship works. The chronic inflammation caused by periodontal disease interferes with your body’s ability to process insulin effectively. This makes blood sugar control more difficult and can accelerate the development of diabetic complications.
Key oral bacteria have been identified as contributing factors to metabolic syndrome, which includes:
- High blood pressure
- High blood sugar
- Excess body fat around the waist
- Abnormal cholesterol levels
Unfortunately, people with diabetes are also more susceptible to infections, including gum disease, because high blood sugar provides an ideal environment for bacteria to flourish. This creates a cycle where poor oral health and diabetes continuously worsen each other.
The good news is that treating gum disease can actually improve blood sugar control in people with diabetes, making oral care an essential component of diabetes management.
Alzheimer’s Disease: The Brain-Mouth Connection
Emerging research reveals alarming connections between your oral health and brain function that researchers are still working to fully understand. The inflammatory processes that begin in your mouth can potentially reach your brain, contributing to neurodegeneration and cognitive decline.
The mechanism involves harmful bacteria from periodontal disease entering your bloodstream and potentially crossing the blood-brain barrier. Once in brain tissue, these bacteria and the inflammatory response they trigger may contribute to the development of Alzheimer’s disease.
Recent studies have found that people with chronic gum disease show:
- Faster cognitive decline
- Higher rates of dementia
- Increased inflammation markers in brain tissue
- Changes in brain structure similar to those seen in Alzheimer’s patients
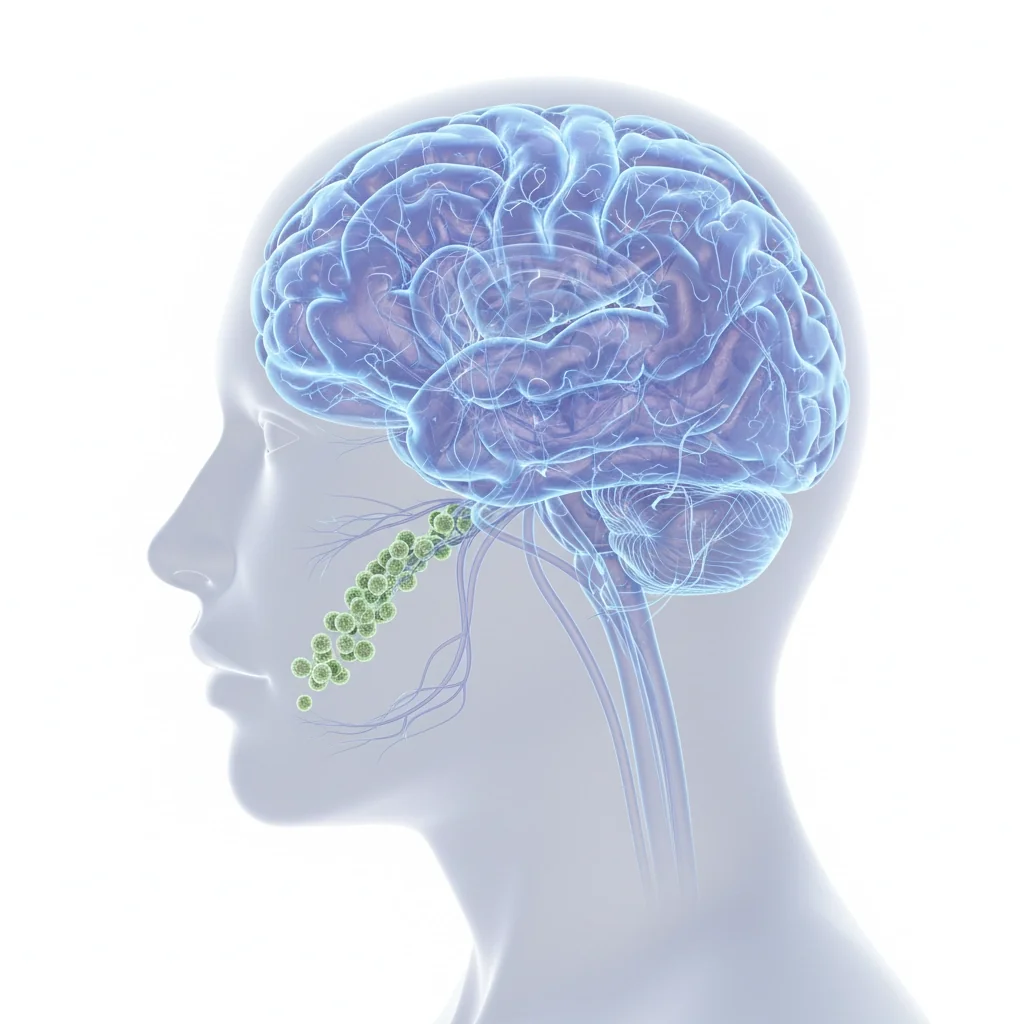
Particularly concerning is the discovery of oral bacteria in the brain tissue of Alzheimer’s patients. While researchers are still determining whether poor oral health directly causes Alzheimer’s or simply accelerates existing conditions, the connection is strong enough that maintaining good oral hygiene is now considered a potential strategy for preserving cognitive function.
Cancer: When Inflammation Becomes Dangerous
Poor oral health significantly increases your cancer risk through multiple pathways, making your mouth both a detection site and a contributing factor for various forms of malignancy. The chronic inflammation and bacterial exposure associated with gum disease create an environment that can promote the cellular changes leading to cancer.
The connection works through several mechanisms:
- Chronic inflammation produces free radicals that can damage DNA
- Certain oral bacteria produce toxins that may trigger cancerous changes
- Poor oral health weakens your immune system’s ability to detect and destroy abnormal cells
Research has linked poor oral health to increased risks of:
- Oral and throat cancers
- Pancreatic cancer
- Kidney cancer
- Blood cancers

What’s particularly important is that cancer symptoms can often first be detected during routine dental examinations. Dentists are frequently the first healthcare providers to notice suspicious lesions, unusual growths, or other early warning signs of oral cancers.
This dual role of oral health: both as a risk factor and detection opportunity: makes regular dental care crucial for cancer prevention and early detection strategies.
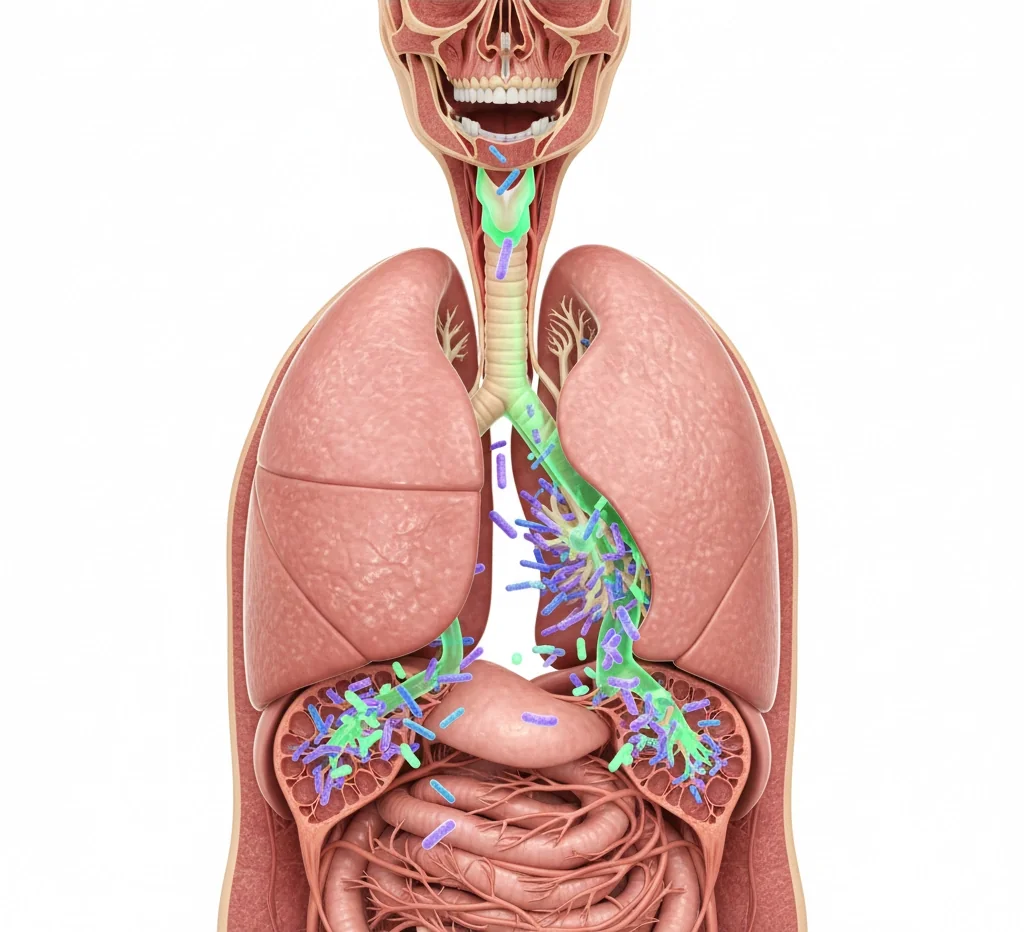
Respiratory Complications: When Bacteria Travel to Your Lungs
Your oral health directly impacts your ability to breathe and fight respiratory infections. Poor dental hygiene creates a reservoir of harmful bacteria in your mouth that can be aspirated into your lungs, causing pneumonia and other serious respiratory infections.
This connection is particularly dangerous for:
- Elderly individuals
- People with compromised immune systems
- Those with existing respiratory conditions
- Hospitalized patients
The mechanism is straightforward but serious: when you have gum disease or poor oral hygiene, your mouth becomes colonized with harmful bacteria. These bacteria can be inhaled into your respiratory system, especially while sleeping, leading to:
- Pneumonia
- Chronic obstructive pulmonary disease (COPD) complications
- Acute respiratory infections
- Worsening of asthma symptoms
Additionally, mouth breathing; often associated with oral health problems, can negatively affect your oral microbiome and create additional respiratory complications. This creates another cycle where respiratory issues and oral health problems reinforce each other.
Understanding the Biological Mechanisms
The connections between oral health and these serious conditions aren’t coincidental. They operate through well-understood biological mechanisms that make prevention possible.
The primary pathways include:
- Bacteremia: Oral bacteria entering the bloodstream through inflamed gums
- Systemic inflammation: Local gum inflammation triggering body-wide inflammatory responses
- Immune system disruption: Chronic oral infections overwhelming and weakening immune responses
- Shared risk factors: Common lifestyle and genetic factors that predispose people to both oral disease and systemic conditions
About 10 specific bacterial species have been identified as key culprits in periodontal disease, with Porphyromonas gingivalis, Actinobacillus actinomycetemcomitans, and Bacteroides forsythus being the most commonly associated with systemic health problems.
Taking Control of Your Health
Understanding these connections empowers you to take control of both your oral health and your overall wellness. The good news is that preventing these serious complications often starts with basic oral hygiene practices that everyone can implement.
Simple steps like daily brushing and flossing, regular dental cleanings, and prompt treatment of gum disease can significantly reduce your risk of developing these life-threatening conditions. When you consider that poor oral health could contribute to heart disease, diabetes complications, cognitive decline, cancer, and respiratory problems, investing in dental care becomes one of the most important health decisions you can make.
If you’re experiencing signs of gum disease, such as bleeding gums, persistent bad breath, or loose teeth: don’t wait to seek professional treatment. Early intervention can not only save your teeth but potentially protect you from far more serious health consequences down the road.